
Am Fam Physician. 2024;110(6):572-573
Author disclosure: No relevant financial relationships.
Prescription opioids continue to be commonly used for chronic non-cancer pain, despite inherent risks. Primary care physicians and advanced practice clinicians have been integral to driving change in opioid prescribing, preventing overuse, and reducing risk. The authors of this article assessed the current extent of opioid prescribing using publicly available data to identify which specialties are most likely to prescribe opioids and to what extent.
Opioid prescribing in the United States has gained notoriety due to the rapid rise of opioid use and overdoses in the 1990s, and these trends continue today.1 Although opioids have a role in treating cancer-related pain and certain chronic comorbidities (eg, sickle cell anemia), they have a high potential for misuse and addiction.2 Primary care physicians and advanced practice clinicians commonly treat pain with nonopioid interventions but also prescribe opioids. Opioid prescribing is more common in specialties such as pain management, anesthesia, and physical medicine and rehabilitation.3
Medicare Part-D Prescribers by Provider and Drug data from 2013 to 2020 were used to analyze opioid prescribing patterns among non-hospitalist primary care physicians and advanced practice clinicians who had prescribed Schedule II opioids during a given year. The top 10% of prescribing specialties were identified, and for primary care the breakdown of prescribing patterns was determined. The characteristics of prescribers who had the highest volume of opioid prescribing were also analyzed.
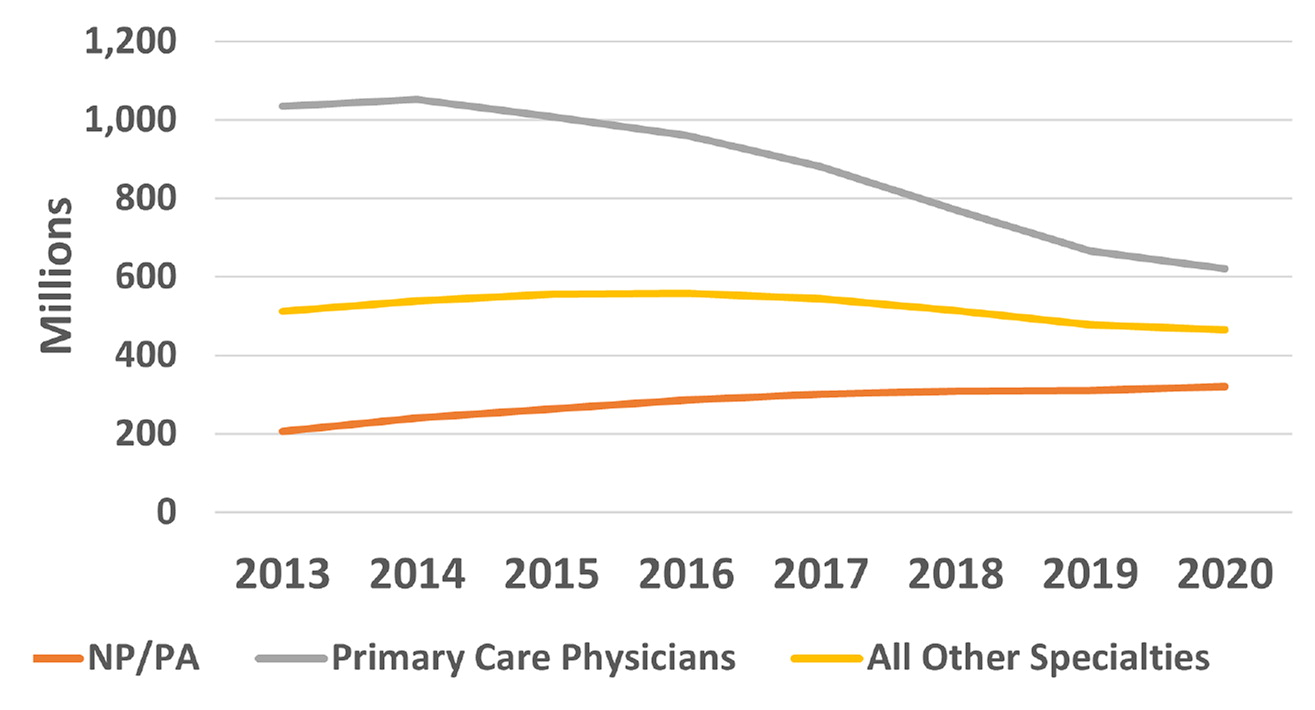
The analysis showed that the total days of opioid prescriptions attributed to primary care physicians declined from 56.9% in 2013 to 43.1% in 2020 (Figure 1). Opioid prescriptions attributed to advanced practice clinicians increased from 11.4% in 2013 to 22.3% in 2020, representing a rise of 6.5% per year in total days supplied. The top third of opioid prescribers had a disproportionate share of primary care physicians and were more commonly located in the South and Midwest. The total number of days of opioids prescribed by primary care physicians fell from 1.03 billion in 2013 to 620 million in 2020, compared with a smaller decline in days of opioids prescribed by all other specialties, from 511 million in 2013 to 464 million in 2020.
The results from this analysis demonstrate that primary care physicians significantly reduced opioid prescribing in alignment with the 2016 Centers for Disease Control and Prevention guidelines, which were updated in 2022.4 Although nearly 7 million US adolescents and adults struggle with opioid use disorder, prevalence is decreasing.5 The use of medications to treat opioid use disorder has increased. The impact of the removal of the X waiver requirement for prescribing buprenorphine in early 2023 has yet to be determined. These findings suggest that the United States is slowly making progress in reducing opioid prescribing in response to the opioid epidemic.
