The cornerstone of this improvement project was a series of clinician focus groups. Here's what they told us about well-being.
Fam Pract Manag. 2024;31(3):23-28
Author disclosures: no relevant financial affiliations.

While significant data exists to demonstrate that clinicians are increasingly becoming burned out, surprisingly little data exists to support interventions to prevent it. Like many organizations, ours has struggled to address the underlying, system-level characteristics that drive clinician burnout and diminish joy in practice.1 So, in late 2019, we created Project Thrive to explore how to best support our clinicians' well-being. The cornerstone of this project was a series of focus groups in which we asked our clinicians for their input, not specifically to uncover “what burns us out” but to illuminate “what builds us up.” In the end, we learned much more than that.
This article shares the steps we followed, what we learned, and what we have done based on the results.
KEY POINTS
In a series of focus groups, clinicians reported that relationships, collaboration, efficiency, adequate time with patients, and innovation bring them joy, while team effectiveness and team members working at the top of their licenses helped them feel accomplished and valued.
Staffing shortages, in-basket volumes, inadequate compensation, poor team dynamics, low levels of autonomy, and administrative burdens were identified as barriers to thriving.
Seeking clinician input on ways to improve their well-being is essential, but organizations must also provide leadership support and take action.
THE FIVE STEPS
Project Thrive is a five-step model that we found to be a simple and effective method to elucidate the supports and obstacles to clinicians' professional satisfaction.
1. Create a project team. Ideally, teams should include clinicians as well as members who have expertise in well-being promotion or quality improvement science.
2. Build a guide for your focus groups to investigate what components of clinicians' work help them thrive. We developed our guide (see the questions below) based in part on recommendations from the Institute for Healthcare Improvement's framework for improving joy in work.2 Questions ranged from “What would make you feel more valued at work?” to “If you could break all the rules, what one thing would you change?”
3. Hold the focus groups. Ours were scheduled for each practice site over lunch or during a monthly clinician meeting, and we invited primary care physicians and advanced practice providers. We held two additional focus groups for clinicians who were unable to attend their clinic-specific session. Attendance was optional. Two clinicians led each focus group, and we held them via a videoconferencing platform for convenience. The focus groups were recorded and later transcribed by an outside company.
4. Review the data in a systematic manner. We suggest using rapid qualitative analysis methods3 to review the data and build a matrix based on how focus group participants answer the questions. Look for emerging themes or agreement for each question.
5. Based on the data, identify what is working well in your practice and areas where changes could improve clinicians' lives and daily work. Define potential actions and partner with practice leaders to implement changes.
WHAT OUR CLINICIANS TOLD US
As our project team reviewed the transcripts for our six focus groups, several dominant themes emerged. For example, when we asked our clinicians what brought them joy, they said relationships, collaboration, innovation, and helping people (specifically, by providing quality patient care). When we asked what helped them feel more engaged at work, they said relationships, having the same team every session, and teamwork. When we asked what would make them feel more valued at work, they said team effectiveness, autonomy, collaboration, relationships, and people respecting their time. (See the full list of questions and themes.)
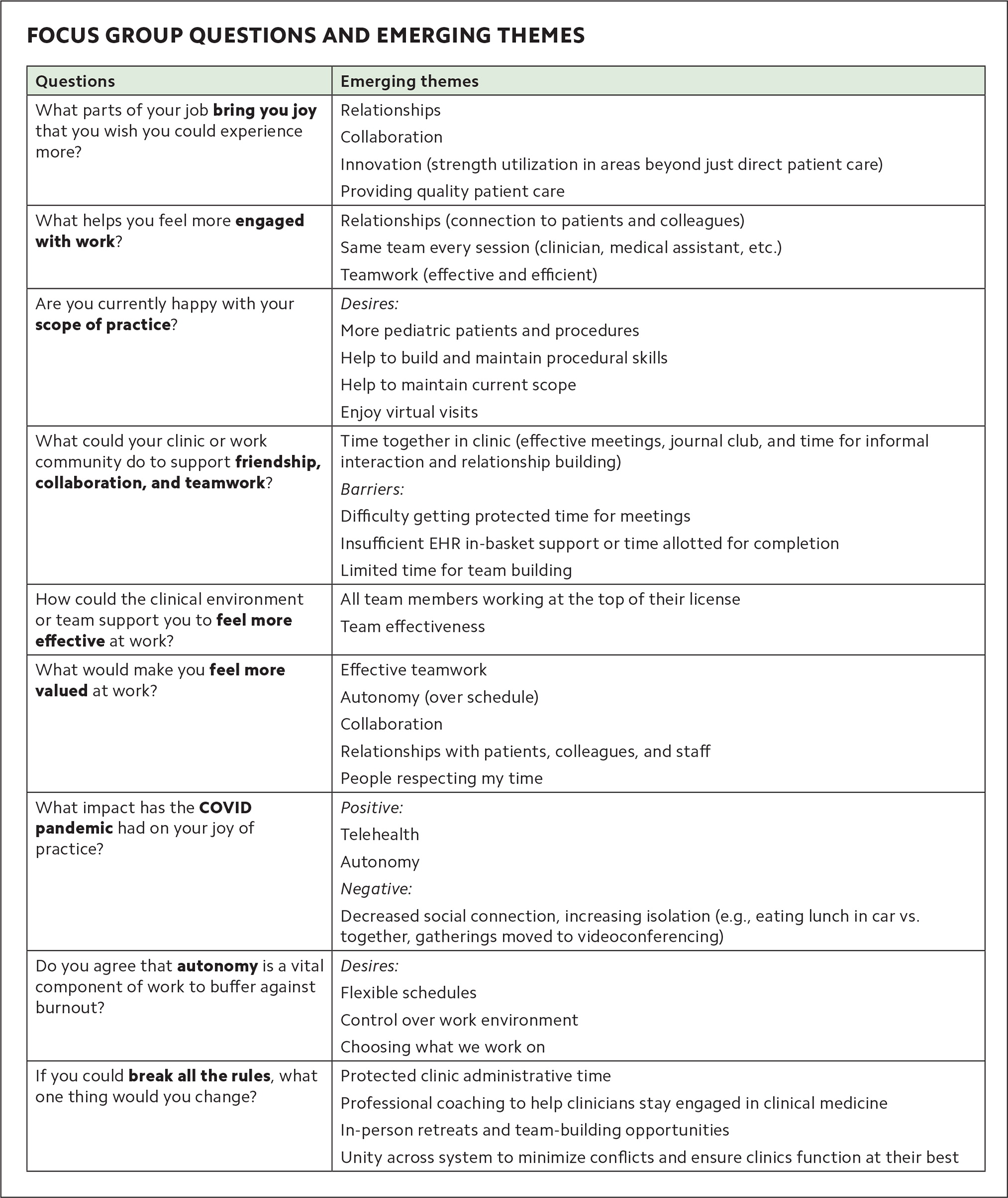
FOCUS GROUP QUESTIONS AND EMERGING THEMES
| Questions | Emerging themes |
|---|---|
| What parts of your job bring you joy that you wish you could experience more? | Relationships |
| Collaboration | |
| Innovation (strength utilization in areas beyond just direct patient care) | |
| Providing quality patient care | |
| What helps you feel more engaged with work? | Relationships (connection to patients and colleagues) |
| Same team every session (clinician, medical assistant, etc.) | |
| Teamwork (effective and efficient) | |
| Are you currently happy with your scope of practice? | Desires: |
| More pediatric patients and procedures | |
| Help to build and maintain procedural skills | |
| Help to maintain current scope | |
| Enjoy virtual visits | |
| What could your clinic or work community do to support friendship, collaboration, and teamwork? | Time together in clinic (effective meetings, journal club, and time for informal interaction and relationship building) |
| Barriers: | |
| Difficulty getting protected time for meetings | |
| Insufficient EHR in-basket support or time allotted for completion | |
| Limited time for team building | |
| How could the clinical environment or team support you to feel more effective at work? | All team members working at the top of their license |
| Team effectiveness | |
| What would make you feel more valued at work? | Effective teamwork |
| Autonomy (over schedule) | |
| Collaboration | |
| Relationships with patients, colleagues, and staff | |
| People respecting my time | |
| What impact has the COVID pandemic had on your joy of practice? | Positive: |
| Telehealth | |
| Autonomy | |
| Negative: | |
| Decreased social connection, increasing isolation (e.g., eating lunch in car vs. together, gatherings moved to videoconferencing) | |
| Do you agree that autonomy is a vital component of work to buffer against burnout? | Desires: |
| Flexible schedules | |
| Control over work environment | |
| Choosing what we work on | |
| If you could break all the rules, what one thing would you change? | Protected clinic administrative time |
| Professional coaching to help clinicians stay engaged in clinical medicine | |
| In-person retreats and team-building opportunities | |
| Unity across system to minimize conflicts and ensure clinics function at their best | |
In addition to answering our scripted questions, clinicians also spontaneously answered the following questions: “What makes your job difficult?” and “What is happening when things are going well?” We did not ask these specific questions, but clinicians naturally shared their thoughts in these areas. We synthesized this information as well (see the tables) to better assess obstacles to full engagement, professional satisfaction, personal accomplishment, and clinic flow.
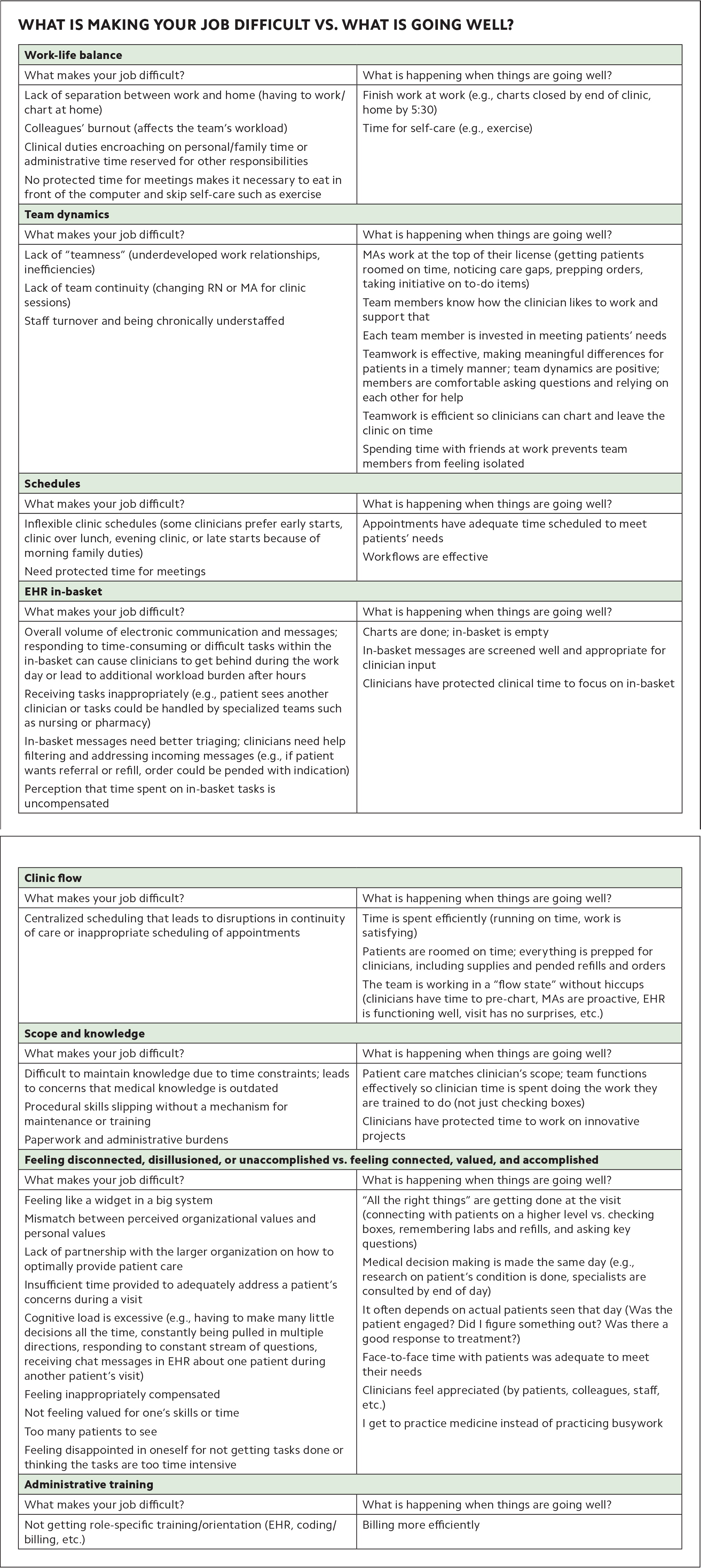
WHAT IS MAKING YOUR JOB DIFFICULT VS. WHAT IS GOING WELL?
| Work-life balance | |
| What makes your job difficult? | What is happening when things are going well? |
| Lack of separation between work and home (having to work/chart at home) Colleagues' burnout (affects the team's workload) Clinical duties encroaching on personal/family time or administrative time reserved for other responsibilities No protected time for meetings makes it necessary to eat in front of the computer and skip self-care such as exercise |
Finish work at work (e.g., charts closed by end of clinic, home by 5:30) Time for self-care (e.g., exercise) |
| Team dynamics | |
| What makes your job difficult? | What is happening when things are going well? |
| Lack of “teamness” (underdeveloped work relationships, inefficiencies) Lack of team continuity (changing RN or MA for clinic sessions) Staff turnover and being chronically understaffed |
MAs work at the top of their license (getting patients roomed on time, noticing care gaps, prepping orders, taking initiative on to-do items) Team members know how the clinician likes to work and support that Each team member is invested in meeting patients' needs Teamwork is effective, making meaningful differences for patients in a timely manner; team dynamics are positive; members are comfortable asking questions and relying on each other for help Teamwork is efficient so clinicians can chart and leave the clinic on time Spending time with friends at work prevents team members from feeling isolated |
| Schedules | |
| What makes your job difficult? | What is happening when things are going well? |
| Inflexible clinic schedules (some clinicians prefer early starts, clinic over lunch, evening clinic, or late starts because of morning family duties) Need protected time for meetings |
Appointments have adequate time scheduled to meet patients' needs Workflows are effective |
| EHR in-basket | |
| What makes your job difficult? | What is happening when things are going well? |
| Overall volume of electronic communication and messages; responding to time-consuming or difficult tasks within the in-basket can cause clinicians to get behind during the work day or lead to additional workload burden after hours Receiving tasks inappropriately (e.g., patient sees another clinician or tasks could be handled by specialized teams such as nursing or pharmacy) In-basket messages need better triaging; clinicians need help filtering and addressing incoming messages (e.g., if patient wants referral or refill, order could be pended with indication) Perception that time spent on in-basket tasks is uncompensated |
Charts are done; in-basket is empty In-basket messages are screened well and appropriate for clinician input Clinicians have protected clinical time to focus on in-basket |
| Clinic flow | |
| What makes your job difficult? | What is happening when things are going well? |
| Centralized scheduling that leads to disruptions in continuity of care or inappropriate scheduling of appointments | Time is spent efficiently (running on time, work is satisfying) Patients are roomed on time; everything is prepped for clinicians, including supplies and pended refills and orders The team is working in a “flow state” without hiccups (clinicians have time to pre-chart, MAs are proactive, EHR is functioning well, visit has no surprises, etc.) |
| Scope and knowledge | |
| What makes your job difficult? | What is happening when things are going well? |
| Difficult to maintain knowledge due to time constraints; leads to concerns that medical knowledge is outdated Procedural skills slipping without a mechanism for maintenance or training Paperwork and administrative burdens |
Patient care matches clinician's scope; team functions effectively so clinician time is spent doing the work they are trained to do (not just checking boxes) Clinicians have protected time to work on innovative projects |
| Feeling disconnected, disillusioned, or unaccomplished vs. feeling connected, valued, and accomplished | |
| What makes your job difficult? | What is happening when things are going well? |
| Feeling like a widget in a big system Mismatch between perceived organizational values and personal values Lack of partnership with the larger organization on how to optimally provide patient care Insufficient time provided to adequately address a patient's concerns during a visit Cognitive load is excessive (e.g., having to make many little decisions all the time, constantly being pulled in multiple directions, responding to constant stream of questions, receiving chat messages in EHR about one patient during another patient's visit) Feeling inappropriately compensated Not feeling valued for one's skills or time Too many patients to see Feeling disappointed in oneself for not getting tasks done or thinking the tasks are too time intensive |
“All the right things” are getting done at the visit (connecting with patients on a higher level vs. checking boxes, remembering labs and refills, and asking key questions) Medical decision making is made the same day (e.g., research on patient's condition is done, specialists are consulted by end of day) It often depends on actual patients seen that day (Was the patient engaged? Did I figure something out? Was there a good response to treatment?) Face-to-face time with patients was adequate to meet their needs Clinicians feel appreciated (by patients, colleagues, staff, etc.) I get to practice medicine instead of practicing busywork |
| Administrative training | |
| What makes your job difficult? | What is happening when things are going well? |
| Not getting role-specific training/orientation (EHR, coding/billing, etc.) | Billing more efficiently |
There was significant consistency among participants from all the focus groups. For instance, they were substantially aligned on the negative impact of staffing shortages, in-basket volumes, administrative burdens, and suboptimal teamwork. Clinicians expressed frustration about having limited opportunities to participate in the greater organization's decisions about patient care and workflows and wanted more autonomy over their practice and schedules. However, what was also clear from the data was the fulfillment clinicians experienced when they could foster work relationships, maximize efficiency, spend adequate time with patients, and feel part of a team that was connected and working well together.
MOVING FROM IDEAS TO ACTION
After examining both lists — what makes clinicians' jobs difficult and what makes things go well — we identified a list of actionable items. We found that the information shared in focus groups was often negative, involving inefficiencies and frustrations about work. Our impression was that people were so disillusioned, burned out, or stretched thin because of significant time pressures and cognitive loads that it was difficult for them to focus on solutions and make innovative recommendations in the moment. For example, some of the focus groups were held over lunch, so clinicians were struggling to finish their morning clinic, make the meeting, and eat while being asked to be innovative. Participants also remarked on the financial obstacles to innovation, recognizing that change requires resources and broader system-level support, which can make improvements inaccessible or frustratingly slow. We know that when people are pressed for time and energy, and are giving everything they have to complete the tasks right in front of them, they may have difficulty thinking creatively and expanding their perspective to include the what-ifs.4 For example, “What if someone helped me with my in-basket? How would I optimize that type of support?”
LIST OF ACTION IDEAS
Provide opportunities to build relationships and “teamness” — both informal (e.g., opportunities to eat lunch together) and formal (more effective team meetings)
Offer professional coaching to help clinicians stay engaged with work (combating burnout, CME planning, time management, etc.)
Identify specialty needs for each clinic and invite physicians to become local experts (to include enhanced training)
Reduce EHR in-basket burden
Create pathways for clinicians to improve patient care and professional fulfillment
Proactively hire staff and improve pay to decrease turnover and promote robust, consistent staffing
Hire a billing coach
Provide reimbursement for answering questions patients send through the EHR portal (may require education on coding for digital E/M services)
Make changes to centralized patient scheduling to improve continuity and appropriate appointment length
Establish a process for clinicians to develop and maintain their procedural skills
Provide opportunities for CME, journal club, and training during clinic to enhance medical knowledge
After reviewing and synthesizing all of the responses, our project team met with the clinic medical directors and department leaders for a half-day retreat where we presented the proposed wellness initiatives, and leaders contributed additional ideas. After small-group discussions, we voted on the top five wellness initiatives that were within the scope of our department. These included the following:
1. Reducing in-basket burden — identify and fix inefficiencies in electronic in-basket workflows to make it easier for clinicians to answer messages and manage tasks.
2. Clinician coaching — hire professional coaches to deliver an evidence-based program, with an optional four-month program available for all clinicians, including the behavioral health team.
3. The “happy place” — support clinicians to focus a portion of their clinical time in professional areas they are most passionate about (e.g., group visits, mental health, research).
4. Planned care — streamline the ordering of health maintenance labs and procedures so clinicians have more time to focus on direct patient care.
5. Empowering the frontline to innovate — support innovation by defining a clear process for clinicians to communicate impactful ideas to leaders and improving clinic-wide communication about innovative projects underway in order to enhance collaboration.
IMPORTANT TAKEAWAYS
A striking observation from our focus groups was that most clinicians have little capacity to look beyond the next patient on their schedule or the tsunami of in-basket messages. They arrive early to avoid being behind before the clinic day even starts, and they frequently leave the office late without the satisfaction of their work being complete. Intellectual real estate for innovation is overtaken by the never-ending to-do list. The unintended consequence is that clinicians are pushed to keep pace on the treadmill and challenged to find the cognitive space or time to think creatively about improving clinic workflow, professional satisfaction, or engagement. This limits clinicians' capacity to dream big, seek out creative solutions, fulfill their mission for medical practice, and apply their strengths in meaningful ways outside the exam room.
Despite the barriers to thriving and satisfaction in clinical practice, clinicians continue to believe that providing high-quality health care services is possible through efficient teamwork, collaborative relationships, support to work at the top of their license, and opportunities to build and maintain meaningful relationships with patients. Our project showed that clinicians want to maximize their time, strengths, and skills to provide quality patient care. Notably, clinicians were asking for practical, realistic changes that could largely be addressed at the clinic and departmental level. Examples include increased opportunities for procedural skill building, medical education training, and professional coaching.
Creating a setting where clinicians could voice concerns and suggest potential solutions was an integral part of the change process. However, we believe the utility of this project was not only asking clinicians questions about their well-being but also having leadership support to implement their ideas.
Organizations should provide ongoing system-level support of clinician well-being in three ways. First, make professional fulfillment a central mission of the organization so that clinician well-being is always a consideration when developing workflows, scheduling meetings, building schedule templates, etc. Second, appoint a wellness leader to coordinate, communicate, and evaluate the organization's initiatives aimed at improving clinician well-being. Third, invest in an initiative like Project Thrive to convey to clinicians that their input is valuable and their concerns are being taken seriously. This approach can help practices identify opportunities for improvement while increasing clinicians' satisfaction, sense of engagement, and capacity to innovate.