
Am Fam Physician. 2024;110(2):116B
Author disclosure: No relevant financial relationships.
To the Editor:
Groin hernias are one of the most common surgical conditions evaluated by primary care physicians, with 1.6 million cases diagnosed and 500,000 surgeries performed annually in the United States.1 Diagnosis is made by obtaining a thorough history and performing a clinical examination of the groin; the latter has a sensitivity of 74.5% and specificity of 96.3%.2
Imaging is often performed despite the recommendation that a groin hernia diagnosis should be predominantly based on physical examination, according to international guidelines adopted by the American Hernia Society.3 Ultrasonography, computed tomography, or magnetic resonance imaging may be a useful diagnostic adjunct, specifically in detecting femoral hernias or symptomatic occult hernias, which are undetectable by physical examination alone.4 However, a recent U.S. study showed that almost 50% of patients planning to undergo surgical evaluation for groin hernia repair had unnecessary preoperative imaging.5 A Canadian study showed that more than 70% of patients with groin hernia had ultrasonography performed before surgical consultation, and only 1.5% of those cases resulted in surgery based on the findings.6 Imaging of the groin for hernia diagnosis and interpretation of the findings generate significant costs and an unnecessary burden to the health care system.
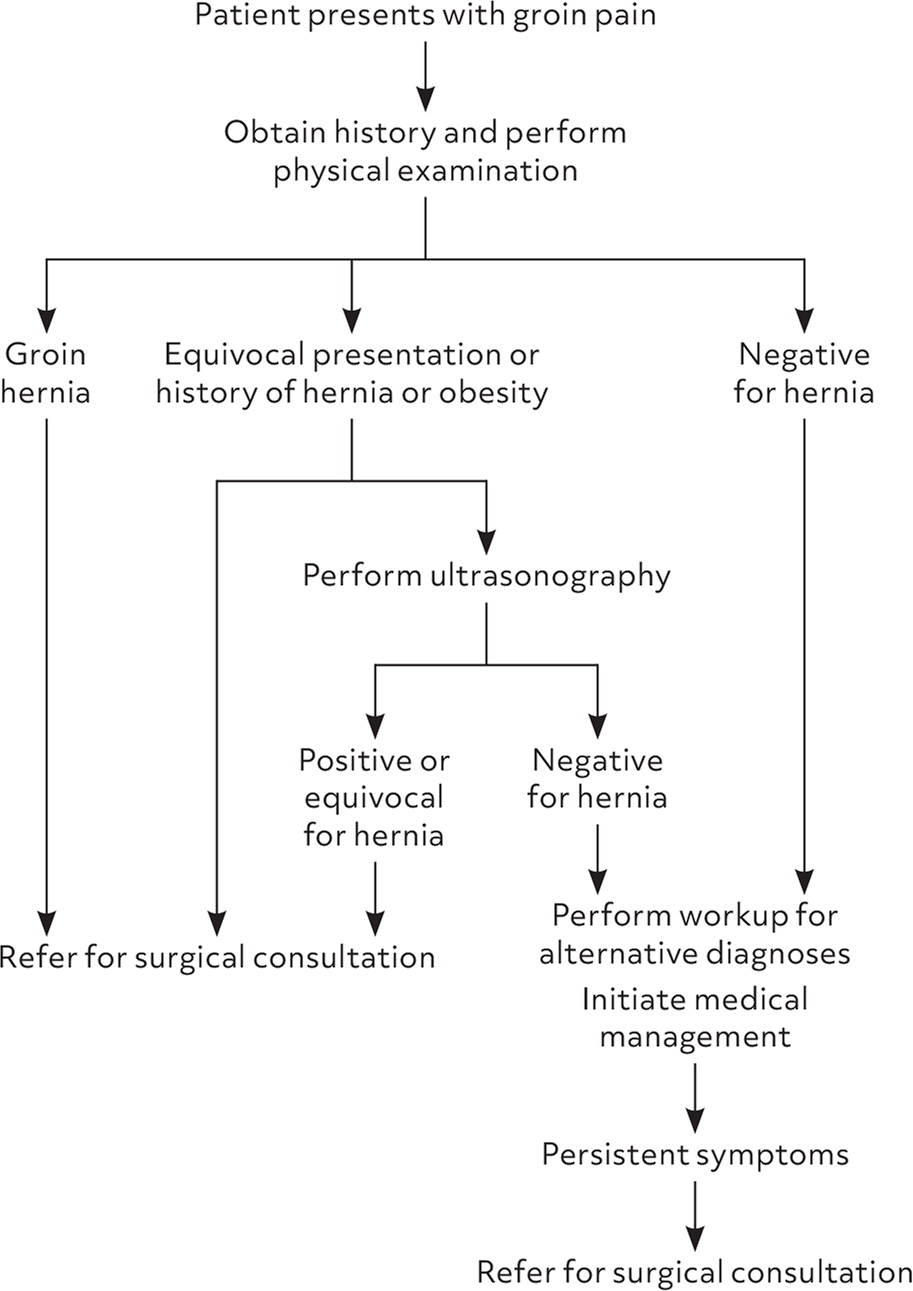
Choosing Wisely guidelines from the Society of American Gastrointestinal and Endoscopic Surgeons recommend against the routine use of imaging for the diagnosis of clinically apparent groin hernias. Fundamental tenets of groin hernia care include obtaining a thorough history, performing a clinical examination, and early surgical consultation. In cases of diagnostic uncertainty, early referral to surgery is warranted. The surgeon should determine the best imaging modality. Positive imaging results alone rarely determine whether patients undergo surgery; therefore, surgeons may diagnose alternative causes of groin pain (Figure 1).
As high costs substantially impede access and reduce equity for patients with fewer financial resources, a “less is more” approach to the diagnosis of groin hernia would have positive impacts on patient care.
