Reopening your practice during COVID-19: where to begin
Although primary care practices are beginning to reopen in many parts of the country, a return to “business as usual” is a long way off, if it’s even possible. New workflows and other changes are now critical to maintaining social distancing and keeping facilities clean and safe. But where should practices begin?
The Centers for Disease Control and Prevention recommends continued use of telehealth to reduce the risk of SARS-CoV-2 transmission, and use of nurse-directed triage protocols to determine if an in-person appointment is necessary. Anyone entering the practice should be screened for signs and symptoms of COVID-19 so that appropriate precautions can be taken.
For Natasha Bhuyan, MD, and colleagues in their Phoenix-based practice, these additional changes have been key to reopening:
- Touchless entry (via automatic doors, propping doors open, etc.),
- Masking all patients,
- Disinfecting rooms with Environmental Protection Agency-approved disinfectants in between each patient visit,
- Adequate personal protective equipment for staff (see “Amazon Gives FPs Priority Access to COVID-19 Supplies”),
- High-efficiency particulate air (HEPA) filters in all exam rooms, lab rooms, and lobby spaces,
- Hand sanitizer everywhere.
Another critical step is redirecting patient flow to promote social distancing. James Dom Dera, MD, and colleagues in Fairlawn, Ohio, functionally removed their lobby/waiting room and added a barrier and signs to redirect traffic through the practice. Because the practice has only one entrance and exit, the office doors are now locked. Patients must call to be let in when they arrive, and are then escorted directly to an exam room. Staff members also escort patients out of the practice, making sure that other patients aren't in the hallway so that incoming and outgoing patients do not cross paths and contaminate each other.
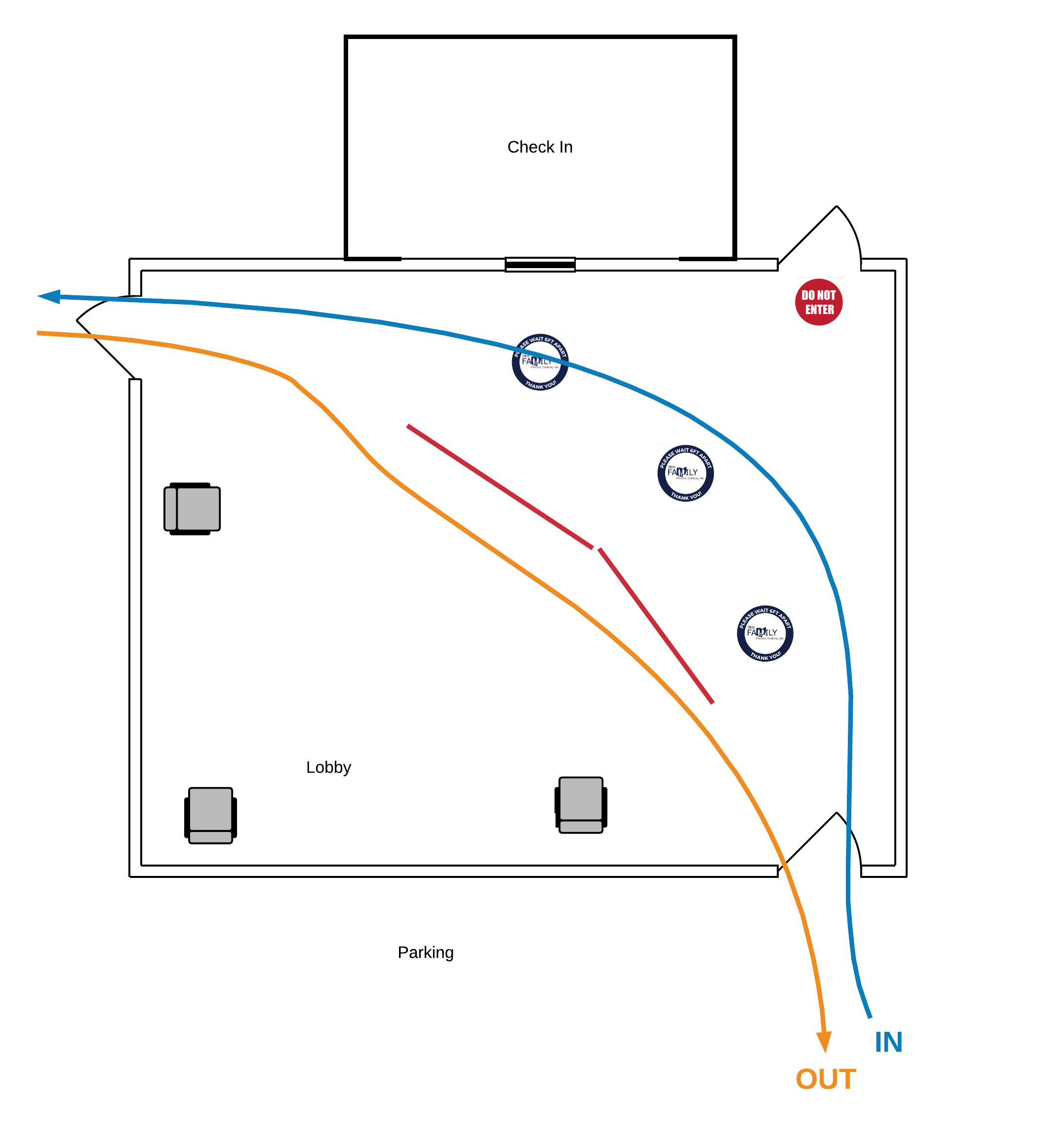
Dom Dera used a spaghetti diagram to analyze the patient rooming and lobby workflow, looking for areas of major intersection. He then remapped the process to address any points of congestion, as shown below.
A spaghetti diagram (above) helped James Dom Dera, MD, identify points of congestion in patient flow and then redesign the process. A barrier and signs (below) now redirect traffic, keeping incoming and outgoing patients from crossing paths.
Get "Quick Tips" in your inbox
Sign up to receive FPM's free, weekly e-newsletter, "Quick Tips & Insights," featuring practical, peer-reviewed advice for improving practice, enhancing the patient experience, and developing a rewarding career.
Other Blogs
- Getting Paid from FPM journal
- AFP Community Blog
- AAFP Voices Blog
Disclaimer: The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. All comments are moderated and will be removed if they violate our Terms of Use.